Understanding the Menstrual Cycle: what all women need to know
For many of us, our knowledge of the menstrual cycle came from biology lessons at school (focussed mainly on reproduction), and from what our mothers or friends told us in our teens – and that may have left us with little or no understanding of the hormones involved, what they do, and when. Or even what a ‘normal’ cycle should be like.
That may be fine when everything is running smoothly! With consistent, regular cycles and few or mild pre-menstrual symptoms.
But that isn’t the experience of periods for many of us….and when things start to change during our perimenopausal years, any gaps in our knowledge can make understanding the changes, and symptoms, much more difficult.
So here is the lowdown on your menstrual cycle; what happens during your cycle, and what is the role of your hormones? What is a normal period? And what isn’t. What symptoms require investigation, and how should you go about getting help?
Before we start, here are a few facts and figures on why this information is SO important:
· Most of us will spend around 40 years of our life menstruating
· Up to 50% of women will experience some kind of ‘menstrual disturbance’ which means period issues or symptoms.
· 1 in 20 women aged between 30 and 49 will see their GP with period related symptoms
· Menstrual issues are still pretty taboo; there is a widely held belief that period problems are just something we should ‘put up with’.
So let’s dive in….
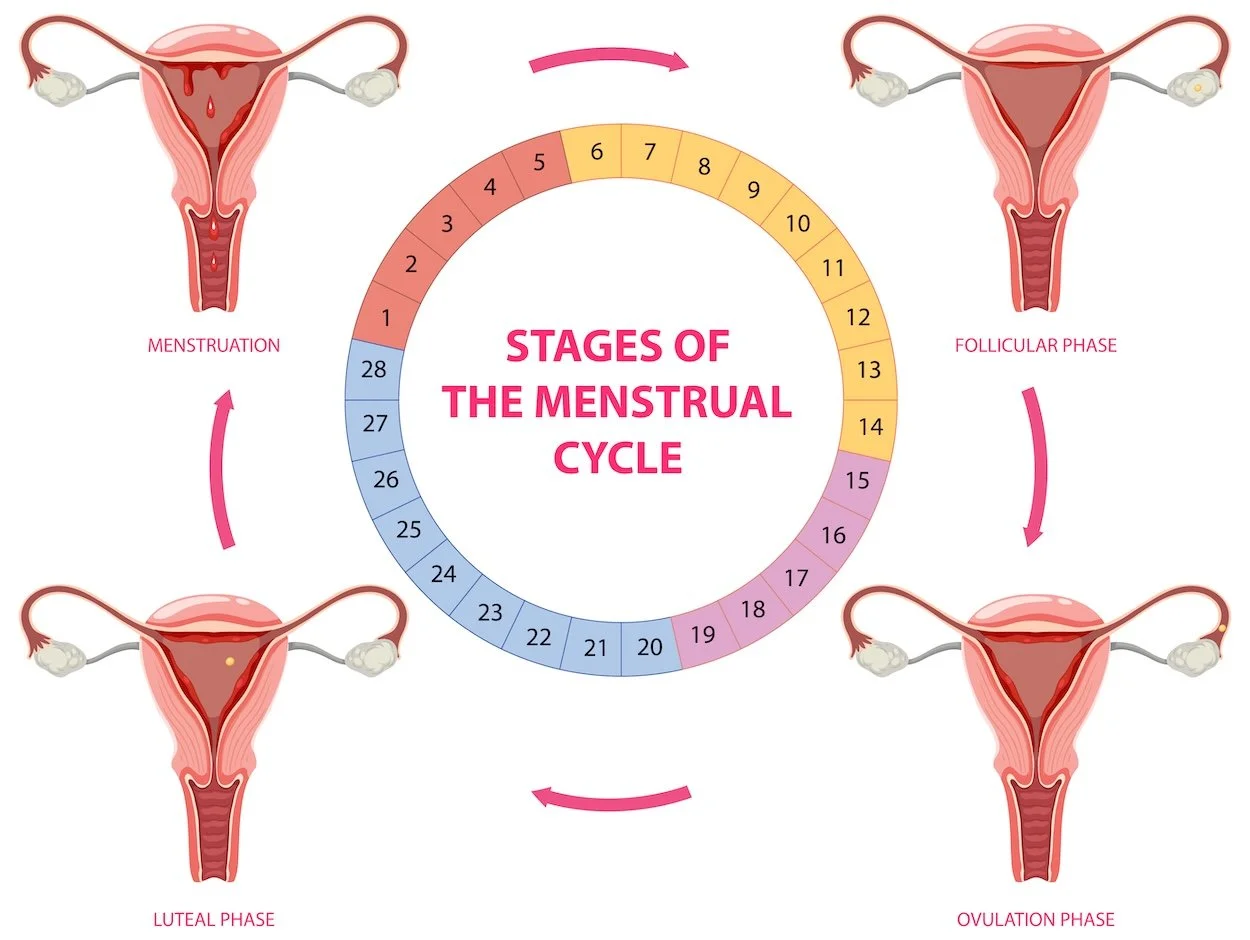
Image Courtesy of FREEPIK
The menstrual cycle
The menstrual cycle is a finely tuned rhythm of hormonal changes that prepares the body for the possibility of pregnancy each month. On average, it lasts about 28 days, though cycles can be shorter or longer depending on the individual. Between 3-5 weeks is normal - and it normal for cycle length not to be exactly the same each month. The period or bleed usually lasts for 2 to 7 days, and again this varies between women. Throughout the cycle, the two key reproductive hormones—oestrogen and progesterone—rise and fall in carefully coordinated patterns, driving the physical and emotional changes many women notice across their cycle.
A cycle starts on Day 1 of your period, which is the beginning of the Follicular Phase, the first half of the cycle. Oestrogen levels gradually increase as follicles in the ovaries mature. This rise in oestrogen helps to build the womb lining so it is ready to accept a fertilised egg.. At ovulation (the release of a mature egg from the ovary) oestrogen levels are at their peak. You might notice a rise in libido or a change in vaginal discharge at this point of your cycle.
During this period of rising oestrogen, nature wants us to go out and find a mate, and to get pregnant! The oestrogen gives most women feelings of increased energy, focus, and even elevated mood. We have lots of get up and go!
Following ovulation, the Luteal Phase begins, and progesterone takes centre stage. Produced by the corpus luteum (the structure left behind in the ovary after ovulation), progesterone thickens the lining of the womb, ready to receive a fertilised egg. During this phase, progesterone levels rise sharply while oestrogen remains present at moderate levels. This shift often brings about noticeable changes, such as a calmer but sometimes more sluggish mood – effectively nature is telling you to slow down, and nest, in case an egg has implanted and you are pregnant. Women often notice pre-menstrual symptoms during this time such as bloating, or breast tenderness. You may also notice increased mood lability, feeling more tearful, low or irritable, again a response to the rising progesterone levels.
If pregnancy does not occur, both progesterone and oestrogen levels drop toward the end of the luteal phase, leading to the shedding of the womb lining—menstruation (your period)—and the cycle begins all over again.
In short, it is normal for women to feel different through their cycle, both mentally and physically. Understanding your own cycle, and how you feel at different points during it, may allow you to plan your time and activities in a way that suits these different phases, or at least to be prepared and to deal with them more effectively.
It is also normal for periods and the menstrual cycle to be irregular when they start (at puberty), and when they start drawing to a close (around perimenopause).
When do periods usually start?
For most girls, periods begin between the ages of 9 and 15. The first period is called menarche, and it marks the start of reproductive capability, though cycles may be irregular for the first few years as the body adjusts to hormonal changes. Genetics, nutrition, body weight, and overall health all play a role in determining when menstruation begins. For example, girls who are very active in sports or who have lower body weight may start a bit later, while those with a higher body fat percentage might start earlier.
The timing of a first period is closely linked to the body’s natural hormonal development. In the years leading up to menarche, the brain’s hypothalamus and pituitary gland begin to signal the ovaries to produce oestrogen. This is responsible for the development of breasts, the growth of pubic and underarm hair, and the start of ovulation. Once the ovaries release eggs regularly, periods begin.
It’s also important to know that starting a period earlier or later than friends isn’t unusual. Everyone’s body has its own pace, and what’s considered "normal" spans a wide range. However, if a girl hasn’t had her first period by age 16, or if her periods start before age 8, it’s a good idea to consult a healthcare professional to make sure development is on track.
When do periods usually end?
Just as there is a natural age range for the first period, there is also a typical time when periods come to an end. Menopause is officially the moment in time when a woman has gone 12 months without a period, marking the end of her reproductive years, in the UK this usually happens between 45-55, with the average age being 51. Medical treatments, such as chemotherapy or surgery to remove the ovaries, can also bring on menopause sooner.
Medical treatments, such as chemotherapy or surgery to remove the ovaries, can also bring on menopause sooner.
The years leading up to menopause are known as the perimenopausal phase. During this time, female hormone levels—especially oestrogen—begin to fluctuate more unpredictably. Periods may become lighter or heavier, shorter or longer, and less regular. Some women experience significant menopausal symptoms such as hot flushes, night sweats, mood changes, or disrupted sleep during this transition, while others notice only subtle changes.
Just like the start of menstruation, the timing of menopause is influenced by a mix of factors, including genetics, lifestyle, and overall health. Some women naturally reach menopause earlier, while others continue menstruating into their late-50s.
What’s normal, and what’s not?
There is still, even now, a huge amount of taboo around menstruation. These taboos can lead to feelings of shame, secrecy or embarrassment prevent women from talking about their menstrual health. Or they may have been conditioned to believe that they should just be able to get on with it and cope, whatever their cycle throws that them. And that means that many women suffering from menstrual disturbance or problems with their periods may struggle along for years before seeking help.
Any woman experiencing the following symptoms should always seek help from a medical professional:
Irregular bleeding: infrequent or absent cycles, very frequent cycles or bleeding between periods
Heavy bleeding: needing to double up or change sanitary wear less the 2 hourly, having large clots or leaking through sanitary wear.
Pain: painful periods that stop you doing things, pain during sex or pain when urinating or opening bowels
Cyclical Mood changes: Feeling emotionally unstable and tearful, persistent low mood, irritability, anger or thoughts of self harm.
Let’s look at each of those in a bit more detail….
Irregular Bleeding
Irregular bleeding is a cycle that either is less than 21 days, or over 5 weeks, or one that just has no regular pattern! (except in puberty, or perimenopause). It would also be a concern if periods were to suddenly stop or change, or if a woman experiences bleeding between periods. If you’re not sure it can be helpful to use an app to monitor your cycle.
Heavy Bleeding
A normal amount of period blood is 30 – 40 mls, which is about 6-8 teaspoons, this can be hard to judge, NOT normal is:
Needing to change pads, tampons or other sanitary products more frequently than every couple of hours for several hours,
Needing to get up in the night to change sanitary products after the first night of your period
Passing large clots of blood (bigger than a 50 pence)
Flooding (sudden gushes of blood causing you to leak through clothing)
Bleeding that lasts longer than 8 days
Iron deficiencies & anaemia
Any time that period bleeding is getting in the way of your life, you should always talk to your doctor.
Pain
It is fairly usual to have some cramping pain in the 24 hours before your period, and during the first 1-2 days after your period starts, but that pain should be relieved by regular painkillers.
It is not normal to have pain during the week before your period, any pain that is so severe that it stops you doing things, makes you feel sick, causes pain during sex, or pain when opening your bowels or urinating.
Mood changes
Mood symptoms that occur in relation to your cycle, normally in the second half may indicate PMS (Pre Menstrual Syndrome). These can range from feeling upset or angry to depression, anxiety, irritability, trouble sleeping, excessive tiredness and suicidal thoughts. Severe PMS is a life changing condition for the sufferer and those around them, this may also be called PMDD (Pre Menstrual Dysphoric Disorder), originally an american medical term. The key is that symptoms are minimal or completely resolve, with or shortly after the start of your period and that they have been persistent with most or all periods within the past 12 months.
When should I seek help with my periods?
The best rule of thumb to use; if your symptoms are affecting your ability to live your life as you want to, and to carry out normal activities, then talk to your doctor, if your doctor doesn’t listen - talk to another doctor, this is not normal and most conditions are highly treatable.
How will my doctor diagnose a menstrual condition?
Your doctor will start by asking lots of questions and taking a full medical history. They may want to examine your tummy or carry out a pelvic examination. A transvaginal ultrasound may be used to look for abnormalities. Blood tests may also be carried out.
It is really helpful if you can be prepared for your appointment, by gathering as much information as possible about your cycle and symptoms. Keeping a diary, or using a period tracking app can be really useful for this. It is really helpful to have a timeline of how your symptoms have developed and any treatments you have tried. If your GP practice offers them, consider using an e-consult; these gather a lot of information that your doctor can use, too.
As well as describing your symptoms, explain to your doctor why you are worried, and what it is you want to achieve. Consider taking someone with you if you feel anxious or emotional – and if you aren’t happy with the outcome of an appointment, do ask to see another doctor.
All images available license free from Unsplash - click on the image to see photographer’s details